
Patient Presentation:
Monica Buffay is a 35-year-old woman who presents to her new PCP with some complaints of feeling tired, lethargic, and “fuzzy-headed” for the last 6 months. When asked about how she has been feeling she uttered “I always feel so tired lately. Maybe I’m working too hard?” . She has seen her previous PCP several times over this period of time, and she has been told that her symptoms are probably due to anemia, depression, or perimenopause. Several months ago, she developed menorrhagia that resulted in iron deficiency anemia (hematocrit 31%, MCV 68 μm3). However despite treatment with iron (and resultant improvement of her anemia), a hormonal contraceptive to help regulate her menstrual cycle, and an antidepressant, her symptoms have slowly worsened. She notes that 24 months ago, she attended a local health fair that provided a variety of laboratory tests. The result of her TSH at that time was 6.2 mIU/L, and her total cholesterol was 246 mg/dL. Her PCP felt that the TSH value was compatible with subclinical hypothyroidism and therefore could not explain her symptoms. She also has noticed that her skin seems more dry and itchy and that she has difficulty keeping warm and frequently wears a sweater, even in warm weather. When asked about her family background, it was found that her father was Positive for CVD, CAD; had Type 2 DM and died of CVA at age 55, her mother is alive with Type 2 DM, HTN, and hypothyroidism and had an MI at 60; she has one brother with Type 2 DM and a sister with HTN.
Her medications were listed as follows:
- MOM 30 mL po daily PRN constipation
- Fluoxetine 20 mg po daily
- Ortho Tri-Cyclen-28 1 po daily
- FeSO4 300 mg po daily
- Calcium carbonate 500 mg po twice daily
- Acetaminophen 325–650 mg po PRN headache, body aches
Review of Systems:
Occasional headaches relieved with non-aspirin pain reliever; (–) tinnitus, vertigo, or infections; frequent body aches which she attributes to lack of exercise; (–) change in urinary frequency, but she has noticed an increase in the number of episodes of constipation in the past year; reports cold extremities; (–) history of seizures, syncope, or LOC, (+) dry skin
Physical Examination
Gen
Well-appearing, middle-aged, Hispanic woman in NAD
VS
BP 142/89, P 64, RR 18, T 36.4°C; Wt 68 kg, Ht 5'4''
Skin
Dry appearing skin and scalp; (–) rashes or lesions
HEENT
PERRLA, EOMI; trace periorbital edema; (–) sinus tenderness; TMs appear normal
Neck/Lymph Nodes
(–) thyroid nodules or goiter; (–) lymphadenopathy, (–) carotid bruits
Lungs/Thorax
CTA
Breasts
(–) lumps/masses
CV
RRR, normal S1, S2; (–) S3 or S4
Abd
NT/ND, (–) organomegaly
Neuro
A & O × 3; CN II–XII intact; DTRs 2+, symmetric
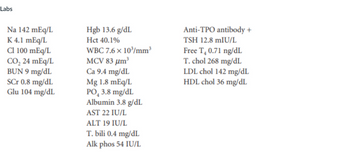
Labs
Assessment
35-year-old woman with signs, symptoms, and laboratory tests consistent with hypothyroidism.
Question:
- Allergies:
- Chief complaint:
- Past medical history:
- Family history:
-
Home medication and dose: Route: Frequency: Last dose (date/time):
Step by stepSolved in 2 steps

- Mr. X is a 64-year-old male admitted to the unit with acute myocardial infarction (AMI) after emergent left (L)-sided heart catheterization/percutaneous coronary intervention (PCI). Past history includes type 2 diabetes mellitus, heart failure, hypertension, andosteoarthritis. Home medications include furosemide (Lasix), digoxin (Lanoxin), captopril (Capoten), carvedilol (Coreg), Byetta (exenatide), metformin (Glucophage), and ibuprofen (Motrin).Clinical AssessmentTwenty-four hours after admission to the unit, Mr. X is alert; oriented to person, place, and time; and pain free. His only complaint is shortness of breath and swelling in his ankles, feet, and hands. Physical assessment reveals bilateral breath sounds with basilar crackles; dressing at catheter site; right femoral clean, dry, and intact; peripheral pulses 2+ bilaterally; and 2+ edema noted in lower extremities. Mr. X has a body mass index (BMI) of 35 kg/m2 and weighs 100 kg. IV fluids have been discontinued, and saline lock…arrow_forwardWhich explanation will the nurse give when a client asks about what causes varicose veins? "Abnormal configurations of the veins." "Incompetent valves of superficial veins." "Decreased pressure within the deep veins." "Atherosclerotic plaque formation in the veins."arrow_forwardCase study : Ms. X, a 32-year-old Hispanic woman, has had a history of intermittent pleuritic chest pain and joint pain for the past several years. Recently, she went to her physician because she noticed that an erythematous, butterfly-shaped rash had appeared on her face. Further lab tests indicated protein in her urine. Her blood test indicated the presence of numerous antinuclear antibodies, especially anti-DNA, and mature neutrophils containing nuclear material. A diagnosis of systemic lupus erythematosus (SLE) was made. Discussion Questions 1. Discuss possible reasons why SLE was not diagnosed earlier 2.Discuss how the presence of antibodies can cause such widespread damage in organ systems. 3. Discuss possible manifestations of SLE 4. Discuss treatments for SLE and a prognosis for the patient in this case.arrow_forward
- A 62-year old, recently widowed male Hispanic patient, KB. was brought in to the emergency department (ED) by his daughter for progressively worsening shortness of breath, fatigue, a lingering non-productive cough, and generalized edema. One month prior, he noticed dyspnea upon exertion, loss of appetite, nausea, vomiting and malaise, which he attributed to the flu. In the emergency department, he appeared anxious and pale, and had a dry yellow tint to the skin. He denied any chest pain, and he could not recall the last time he urinated. He has history of benign prostatic hyperplasia, diabetes mellitus type 2, hypertension, dyslipidemia, and renal insufficiency for the past two years. His ED assessment findings included: 1+ pedal edema, basilar crackles in the lungs bilaterally, and a scant amount of urine according to a bladder scan. His lab results indicated a glomerular filtration rate (GFR) of 12. Based on his subjective and objective symptoms, he was admitted with a diagnosis of…arrow_forwardSituation:Sara Lin is an 18-year-old patient who had an emergency appendectomy. It is day 2 postoperative, and Sara is expected to be discharged late this afternoon. We have discontinued her IV antibiotics after her morning dose. She will be getting oral meds today.Background:Sara presented in the ED 2 days ago with a 2-day history of nausea, vomiting, and increasing pain. She was taken to surgery that day and had an open appendectomy for a ruptured appendix. She has been stable since arriving to the unit. Her parents have been here with her most of the time and are very helpful and supportive.Assessment:Sara is alert and oriented. She needs to be reminded to use her incentive spirometer. Abdomen is soft and tender to touch. Bowel sounds active. She has progressed to regular diet, and she's eating small amounts. No nausea reported since postoperative day 1. The surgery team changed the abdominal dressing early this morning. The incision is closed with staples; the edges are well…arrow_forwardA 42-year-old obese client with complaints of severe radiating chest pain, tightening in the chest, and dyspnea has received a diagnosis of angina pectoris. He is prescribed nitroglycerin tablets to relieve the pain attacks. During a follow-up visit, the client tells the nurse that the frequency and duration of the attacks have reduced with the use of nitroglycerin tablets, and now he is eager to take necessary precautions. The client is also a heavy smoker.a. Why would you say that the client has angina pectoris and not myocardial infarction? b. What instructions should the nurse give the client to prevent further attacks? 11, 12, 132. A 50-year-old stockbroker has recovered from coronary artery bypass grafting (CABG) surgery and is soon to be discharged. He is concerned about possible risks of coronary artery disease (CAD) and wants to lead a healthier lifestyle. What instructions should a nurse give to the client to prevent further CAD? 3. A client is scheduled for an…arrow_forward
- Identifiy one nursing diagnosis each for the left and right sided heart failure.arrow_forwardA 50-year-old female patient, Mrs. Smith, who recently underwent abdominal surgery, is reluctant to ambulate due to pain. She has a history of deep vein thrombosis and is currently on anticoagulant therapy. Her pain score is 6/10 on the numeric rating scale. Options: a) Encourage bed rest until pain subsides. b) Administer prescribed pain medication and assist with ambulation. c) Apply a cold compress to the surgical site. d) Increase the dose of anticoagulant therapy.arrow_forward7) Identify three complications resulting from increased ICParrow_forward
- Pathophysiology: chapter 7: Neoplasia Jane Foster [JF] is a 26-year-old woman in the clinic today for her annual physical examination. As the nurse performs the initial physical assessment, it becomes apparent the client is quite concerned about her risk for developing breast cancer. Her mother and a maternal aunt both developed breast cancer in their late 40s. JF “heard that genetic testing can be done” to see whether she carries “breast cancer genes.” The nurse knows JF is asking about the BRCA1 and BRCA2 mutation genes. What additional information could the nurse share with JF? 1.Explain the role mutation genes have in the genetic mechanisms of breast cancer development.arrow_forwardCase study: Amelia is a 68-year-old woman who was brought into ED by herneighbour. She woke this morning at 0600 hours with a 5/10 headache.At 0700 she called her neighbour and asked her to bring her to hospitalwhen she began to feel weak, and her headache increased to 7/10. Atthis time, one side of her face began to “feel strange”.She has past medical history of Atrial fibrillation (AF), hypertension (HT)and dyslipidaemia which she manages with Apixaban 2.5mg BD, Sotolol80mg daily, Amlodipine 5mg daily, Irbesartan/hydrochlorothiazide300/25mg daily, Rosuvastatin 10mg daily.Amelia used to smoke 20 cigarettes/day but states she quit 5 years ago.When she was brought into ED, she told staff that she did not take hermedications this morning as she was too distracted by her increasingheadache.You are assigned to care for Amelia. As you are about to enter her room,you overhear Amelia crying to her neighbour, explaining that she isworried as her mother had died of a stroke. Vital signs:•…arrow_forwardA client is brought to hospital after being in a car accident. They have lost a significant amount of blood. Their symptoms include tachycardia, pallor, cool skin, and decreased urine output. The nurse understands that these signs and symptoms are a consequence of: Question 20 options: a) The body's normal homeostatic compensatory mechanisms b) Fluid shift to the extracellular space due increased vascular permeability c) The effects of rapidly infused IV fluids administered by paramedics d) Cardiac failure due to pulmonary hypertensionarrow_forward
 Phlebotomy EssentialsNursingISBN:9781451194524Author:Ruth McCall, Cathee M. Tankersley MT(ASCP)Publisher:JONES+BARTLETT PUBLISHERS, INC.
Phlebotomy EssentialsNursingISBN:9781451194524Author:Ruth McCall, Cathee M. Tankersley MT(ASCP)Publisher:JONES+BARTLETT PUBLISHERS, INC. Gould's Pathophysiology for the Health Profession...NursingISBN:9780323414425Author:Robert J Hubert BSPublisher:Saunders
Gould's Pathophysiology for the Health Profession...NursingISBN:9780323414425Author:Robert J Hubert BSPublisher:Saunders Fundamentals Of NursingNursingISBN:9781496362179Author:Taylor, Carol (carol R.), LYNN, Pamela (pamela Barbara), Bartlett, Jennifer L.Publisher:Wolters Kluwer,
Fundamentals Of NursingNursingISBN:9781496362179Author:Taylor, Carol (carol R.), LYNN, Pamela (pamela Barbara), Bartlett, Jennifer L.Publisher:Wolters Kluwer, Fundamentals of Nursing, 9eNursingISBN:9780323327404Author:Patricia A. Potter RN MSN PhD FAAN, Anne Griffin Perry RN EdD FAAN, Patricia Stockert RN BSN MS PhD, Amy Hall RN BSN MS PhD CNEPublisher:Elsevier Science
Fundamentals of Nursing, 9eNursingISBN:9780323327404Author:Patricia A. Potter RN MSN PhD FAAN, Anne Griffin Perry RN EdD FAAN, Patricia Stockert RN BSN MS PhD, Amy Hall RN BSN MS PhD CNEPublisher:Elsevier Science Study Guide for Gould's Pathophysiology for the H...NursingISBN:9780323414142Author:Hubert BS, Robert J; VanMeter PhD, Karin C.Publisher:Saunders
Study Guide for Gould's Pathophysiology for the H...NursingISBN:9780323414142Author:Hubert BS, Robert J; VanMeter PhD, Karin C.Publisher:Saunders Issues and Ethics in the Helping Professions (Min...NursingISBN:9781337406291Author:Gerald Corey, Marianne Schneider Corey, Cindy CoreyPublisher:Cengage Learning
Issues and Ethics in the Helping Professions (Min...NursingISBN:9781337406291Author:Gerald Corey, Marianne Schneider Corey, Cindy CoreyPublisher:Cengage Learning





